Seattle on High Alert as Rare Drug-Resistant Fungal Infection Spreads
An outbreak of Candida auris, a multi-drug resistant fungal infection, has recently been reported in Washington state, raising concerns among health experts due to its high mortality rate, drug resistance, and ability to spread easily in healthcare facilities.
Candida auris, a fungus that grows as yeast, is known for causing severe illness and is typically resistant to antifungal medications, according to the Centers for Disease Control and Prevention (CDC).
Emerging Threat
The Seattle and King County public health department identified three confirmed cases of Candida auris infection, all linked to Kindred Hospital Seattle. The first case was detected through a proactive screening program on January 10, with subsequent cases discovered during the patients’ hospital stay.
Despite initial negative tests upon admission, further testing revealed that the patients had contracted the infection during their hospital stay, highlighting the fungus’s ability to spread within healthcare facilities.
The source of the outbreak has not been identified yet, prompting local officials to work with Kindred Hospital to isolate infected patients and notify facilities that admitted patients from Kindred.
Candida auris has been on the radar of health authorities, with the CDC issuing a warning in May 2023 about an increase in cases spreading in healthcare facilities, labeling it an “urgent antimicrobial resistant threat” In 2022, there were 2,377 reported cases of Candida auris infections in the US, making it a growing concern.
First identified in Japan in 2009, Candida auris cases have been on the rise in the United States since 2016, with a significant increase during the COVID-19 pandemic between 2020 and 2021. The fungus has been reported in 36 states, with the majority of cases concentrated in New York, Illinois, New Jersey, California, and Florida.
Seattle Raise Concerns for Healthcare Facilities
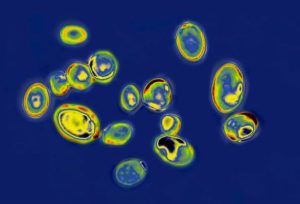
One of the challenges associated with Candida auris is its resistance to antifungal medications, with 90% of strains being resistant to at least one antifungal, and 30% resistant to at least two.
The infection is often misdiagnosed, leading to inadequate treatment, and it can survive on surfaces in healthcare facilities for at least two weeks, contributing to its rapid spread.
Candida auris infections can cause severe illness and hospitalization, particularly in healthcare patients with serious medical issues. The CDC reports that one in three people with an invasive Candida auris infection, affecting areas like the heart, brain, and blood, may succumb to the infection.
The recent outbreak in Washington state highlights the persistent threat of Candida auris and the challenges it poses to healthcare facilities.
The urgent need for effective prevention, diagnosis, and containment measures is emphasized, given the fungus’s high mortality rate and its potential to become a significant public health concern.

